Health
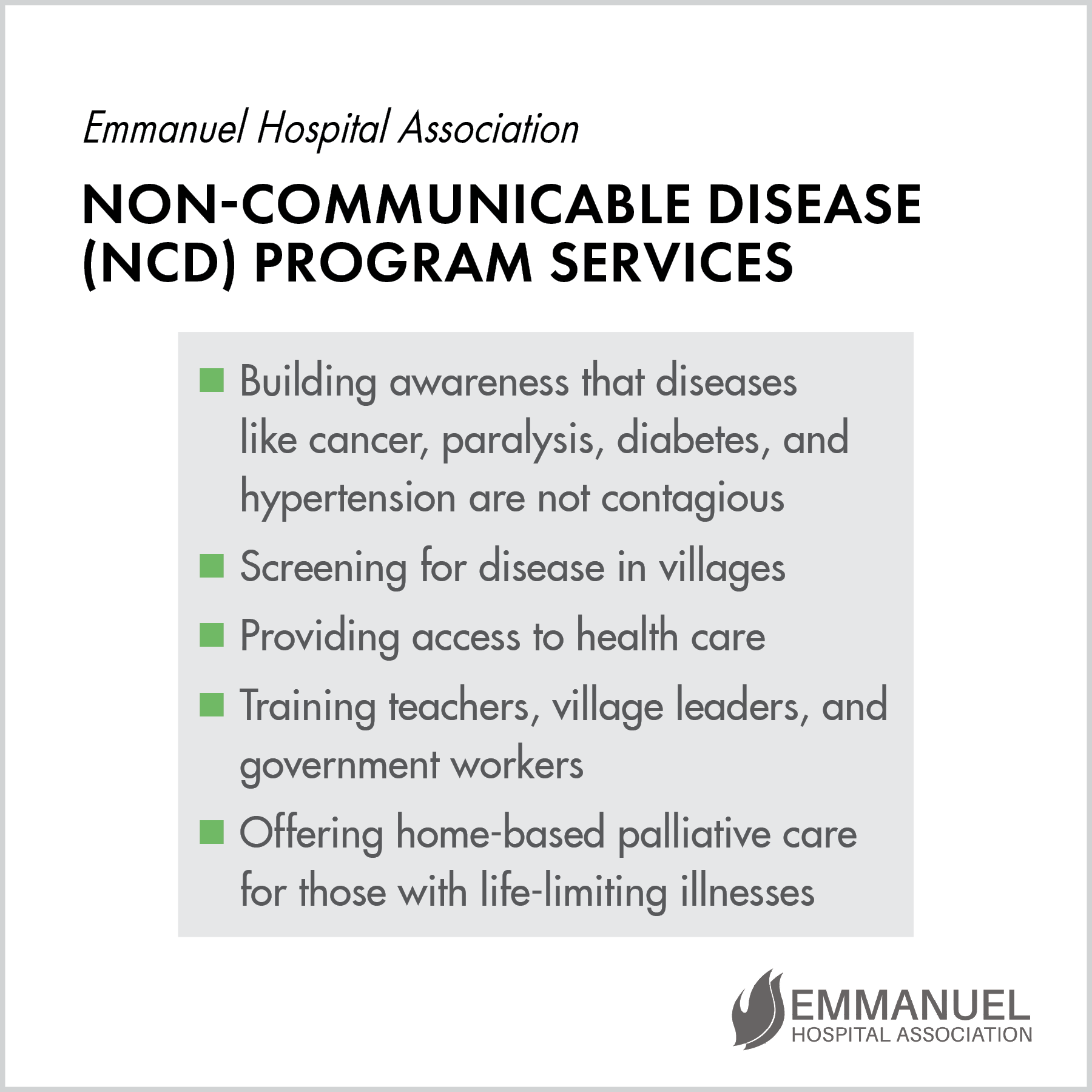
When EHA medical teams go out into the villages, they face an uphill battle. Due to limited education, low literacy rates, and long-held false beliefs, many villagers simply don’t understand much about diseases like diabetes or hypertension or cancer. They don’t know what signs to look for with diseases like these, and they certainly aren’t seeking regular medical checkups. Often they believe that these diseases can be contagious, so they avoid people who have been diagnosed, plunging those who are sick into isolation at the worst time.
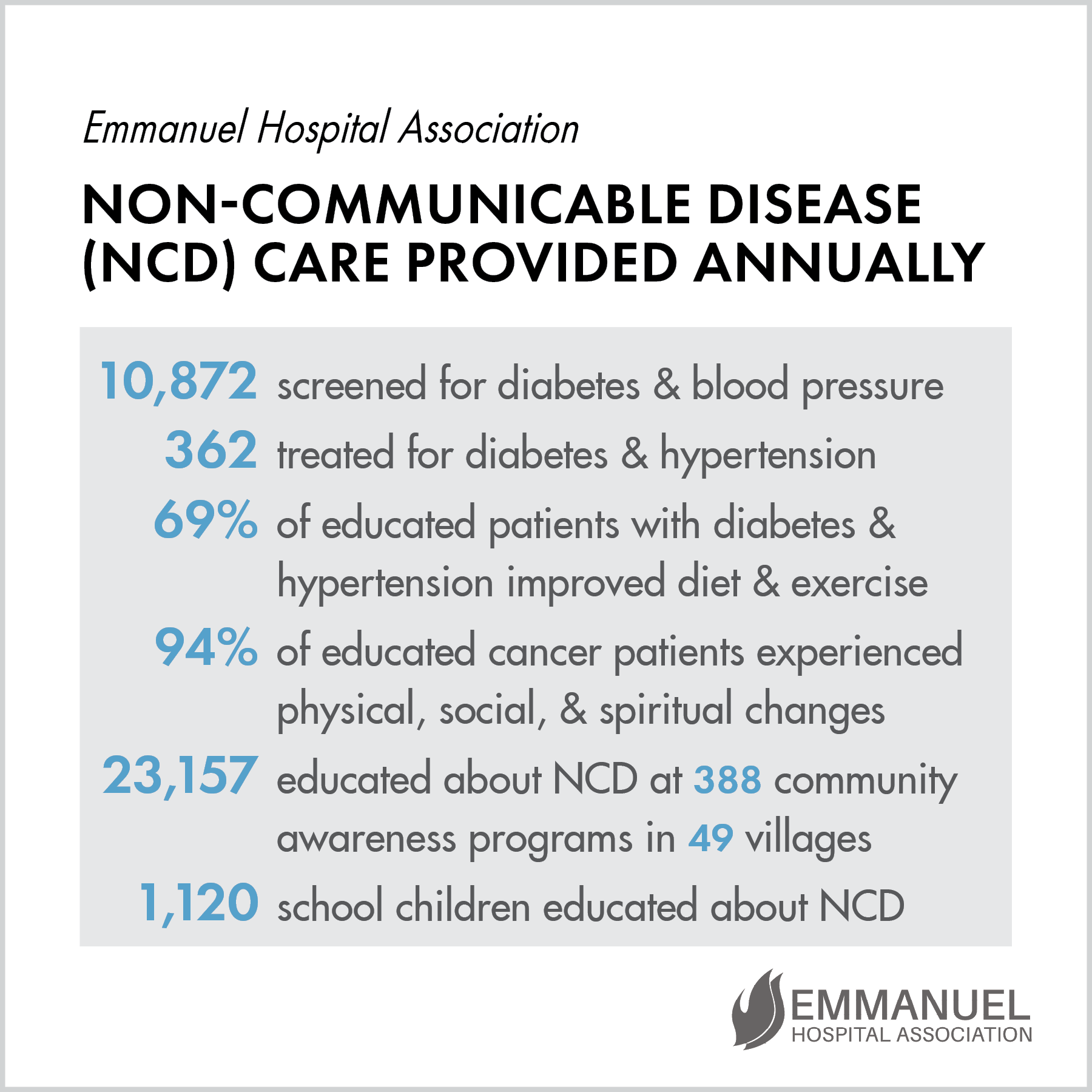
So EHA community teams drive from village to village, providing testing and teaching people more about these diseases. They seek out those in leadership in the villages, including teachers and government workers, and provide training for them in what to look for and how to help people seek treatment. And when they find patients with life-limiting illnesses, the palliative care teams visit patients’ homes, meeting their physical, social, and spiritual needs. They are the hands and feet of God to these people. The charts below explain what they do and the results of their efforts. The articles that follow tell the stories of several people whose lives were changed by the care of EHA’s doctors and nurses.
Kicked Out of the House

When Kabir found out his father, Mukund, had oral cancer, he kicked him out of his house because he feared the other family members would get cancer too. He wanted nothing to do with him, and refused to provide him food or go near him. Mukund began living alone in the neighbor’s shed with the goats and cow. He was afraid that if others in the village found out he had cancer, they would throw him out of the village as well.
Mukund’s pain became so unbearable, he decided to end his life by taking poison. The next day he went to withdraw money to buy poison, but an EHA staff member, Mr. Raj, who knew him began to talk with him. Mukund poured out his story of pain and isolation and confessed his plan to commit suicide. Immediately Mr. Raj counseled and prayed with him, and then called community health staff to come and help. Mukund was reassured that he would be cared for.
The community team brought Mukund to Duncan Hospital, accompanied by Kabir. When the doctor dressed the infected abscess, Kabir was shocked to see him touch the wound. The palliative care team began to visit Mukund regularly to change his bandages and educate the family, and Kabir decided to allow his father back into the house and to care for him. This turnaround is a great blessing to Mukund and a wonderful example to the community.
Breathing Her Last Breath in Peace

When Manju found a small wound on the right side of her chest, she went to a clinic in Raxaul for treatment. When it grew worse, her children took her to a cancer hospital, and the biopsy revealed that she had breast cancer.
Manju’s family lived on the wages from her son’s daily labor at a watch repair shop. They lived in a rented home, and the owner was pressuring them to move out so that her cancer would not spread to others. Her neighbors were also afraid they would catch the disease and refused to visit her.
By the time her son asked an EHA community health team to get involved, Manju was lying on a dirty bed in filthy clothing, suffering from fever. Her pain was unbearable and the wound had grown in size so that she had trouble lying down, getting up, sitting, and sleeping. She felt helpless, was full of despair, and wanted to die.
The team gave Manju a bath, dressed her in clean clothing, and made her bed with fresh coverings. Over many visits they met her physical needs and dressed her wound, and once trust had grown with her family members, the team trained them in how to care for her. They also taught the family how to pray, how to forgive others, and how to apologize. Because of the team’s emphasis on healthy relationships, family rifts were healed.
Once Manju’s wound smelled better, she looked happier, and her daughters-in-law were willing to care for her and feed her. They began cleaning her room and keeping her windows open for fresh air. At the time of Manju’s death, her family members were gathered around her, and she breathed her last breath in peace.
Thanks to the EHA community team’s 30 home visits over time, Manju was able to pass on comfortably and in harmony with her family.
Community Projects Provide Needed Care

Burrows Memorial Christian Hospital (BMCH) organizes health camps in the surrounding communities in partnership with the government, and nearly 1,000 patients were seen by their doctors in the last year. Patients received a checkup and free medicine. The BMCH staff were pleased with the response to these medical camps and plan to hold more in the future.
The lay leader program is also flourishing. For example, Ganga works as a community lay leader in the areas around BMCH in conjunction with the Tripura Baptist Christian Union. She has been trained by hospital staff to examine patients and recommend care. Recently Ganga conducted a health education session and 11 people came to her for advice. One man had a snakebite and she immediately sent him to the hospital. He listened to her and went to the hospital instead of the witch doctor, and he survived. Another person had been bitten by a dog, so Ganga was able to educate him on how to prevent rabies. She diagnosed another man with hypertension and advised him to go to a doctor and learn how to lower his blood pressure. Since Ganga has been helping the people in these communities, it has opened up opportunities for her to share about God.
In other programs, BMCH responded to a request by the Indian prime minister to provide free monthly prenatal checkups to all pregnant women. These women also receive free labwork, ultrasounds, and medicine. BMCH supplied these services to 950 women in the last year.
Village Nurse Training Improves Care

Rama Bharati had been an Auxillary Nurse Midwife for the government for eight years. She worked out of a health center in the village of Padwaha and was supposed to deliver a multitude of services, including immunizations, antenatal and postnatal care, nutrition education, and treatment of minor illnesses. But Rama confined herself to routine immunizations and was not trained in how to do abdominal checkups for antenatal care or follow up visits for postnatal care. She had gaps in her knowledge, attitude, and skills in providing health services to the surrounding people.
Then the Prerana Project staff from Chhatarpur Christian Hospital began to work in Padwaha with the goal of improving the quality of antenatal and postnatal care, the health of children under five, and nutrition services. The Prerana nurses built relationships in the community and with the government health service providers, including Rama. Eventually, Rama was asked by her supervisor to learn from the Prerana nurses and improve her patient care. She began to show an interest in learning new skills, and she gained confidence in each area she was lacking in.
Now Rama is quite happy and confident in her job at the health center. The villagers and her supervisor are both pleased with her efforts to provide proper health care services in Padwaha village, and they appreciate the Prerana nurses’ perseverance in bringing this change about.
Health Education in a Tea Field

It’s a win-win situation. The nursing school students gain experience, and the community gets education in health care issues.
This small Community Health Project out of Makunda Christian Hospital was started in 2006 in the midst of a tea field. Twice a week, nursing students teach villagers on topics such as nutrition, sanitation, and simple treatment for common local diseases. Many of these families struggle with poverty, so malnutrition and lack of healthcare for children are common problems.
Nursing students visit expectant and new mothers to talk about proper, healthy care for young children. Vaccines are provided. School children are also taught, and due to their enthusiastic sharing with their families, the knowledge spreads. This causes the entire village to hear about and think about health issues. One specific issue addressed by this program is the use of latrines.
Before this project began, less than two percent of the villagers used latrines, causing human waste to be a serious sanitation issue. Due to the work of the nursing students providing education about sanitation, 20 percent of the villagers now use latrines. Reaching out with the love of God to make a difference in these villagers’ lives is an integral part in the training of Makunda’s nursing students.
Spreading Medical Care

Each EHA hospital has a Community Health and Development Program (CHDP) that works in surrounding villages to provide medical care. Burrows Memorial Christian Hospital holds medical camps to provide preventative and current medical care in 12 outlying villages. Their vision is to empower these communities to take charge of their medical care and also help them access government programs that provide needed services.
There are many false beliefs and myths regarding medical care, as well as innumerable untrained “doctors” happy to take people’s money for “treatment,” so the CHDP staff hold teaching and awareness programs to educate villagers.
The CHDP staff team also assists with the training of missionaries and evangelists who work in rural areas so that they can provide simple medical care and direct patients to more extensive treatment at the hospital when needed. They teach these missionaries to do screenings for illnesses such as diabetes and high blood pressure. In this way, BMCH is able to spread health and medical care to many more people than just those who walk through their doors.
Community Health Projects Expand

Broadwell’s Community Health and Development Program Department runs several projects to facilitate social and economic transformation in the communities by building capacity, by addressing gaps in the health system, and by providing advocacy.
One project they run involves training laypeople in basic healthcare skills. Since pastors are often out and about taking care of people’s spiritual needs, BCH staff train them in basic healthcare so they can assess needs and help get those who need hospital care in to BCH’s facility.
Another group trained in healthcare are women called Community Health Guide Volunteers, and they are chosen by their communities to serve as their point person for health and development issues. They are trained in basic health and disease prevention, and when they go back into their communities, they are able to help meet the basic healthcare needs of those who are unable or unwilling to go in to the hospital.
They also have a rural project in the Teliyani block that covers 30 villages with a total population of 30,000. After four years of operation, they are starting to see real transformation in the lives of the villagers.
BCH has another project that operates in 15 slums around Fatehpur, focusing on the living conditions of the victims of the caste system. In three years this project has brought about remarkable changes in behavior and awareness, as well as in accessing rights. Often these people have no idea what benefits they are eligible for from the government, and CHDP staff work with them to help them obtain the things they are entitled to.
Through each of these projects, BCH staff are able to improve the living and health conditions of the poor who really need their help.
Reaching Urban Lalitpur

EHA’s Harriet Benson Memorial Hospital has partnered with Lalitpur Bible School to reach out to the community around them. Student interns from the school have carried out a health-issue survey of 900 households in the Azadpura urban area.
One of the key areas they are looking into is non-communicable diseases (NCDs) such as diabetes, heart disease, and cancer. These NCDs are now killing more Indians than the traditionally feared infectious diseases such as TB, HIV, dysentery, and viruses that lead to pneumonia. The challenge in stopping NCDs is that they are linked to lifestyles, and the effect of changing one’s health behaviors takes a long time to see. There are no quick and easy approaches to solving these problems, but people want “a pill for every problem, a needle for every need.”
To address these concerns, Harriet Benson has begun offering both breast cancer and diabetes awareness training, screening camps, and treatment clinics. Each month, they offer eight to twelve screening camps in the surrounding urban areas, and have found at least ten percent of the population to have diabetes. They then refer these patients to the diabetes clinic, where they receive education and treatment.
The National Health mission officer heard about Harriet Benson’s camps and asked them to do screening for the Urban Health Mission clinic that the government runs. Harriet Benson staff gave diabetes education and screened participants along with the government health workers. This collaboration with the government health authorities is excellent for both parties. The hope is that they can collaborate further in the future.
Health Practices Shared

One area where nursing students are a big help is in the Community Health and Development Programs. Burrows Memorial strives to educate the surrounding villages regarding good health behavior practices. They offer education classes on improved nutrition, self care and personal hygiene, and environmental sanitation including the important use of latrines. Nursing students teach some of these sessions, and their care for the villagers is evident. They also visit expectant and nursing mothers to talk about good health care for newborns.
One specific issue addressed by these programs is the use of hygiene regarding toilets. Before this program, few villagers regularly used toilets, practiced hand washing, or bathed with soap. This understandably led to preventable sickness. Due to the tireless efforts of EHA staff and nursing students in providing villagers education on sanitation, health, and hygiene, many people have been inspired to change their living habits. EHA staff are motivated to teach these people practical health behaviors to improve their lives and health.

About Health
Many times, health is about education as much as anything else. Many health programs focus on treating diseases and providing care for sick patients. EHA does that too, of course. But EHA also endeavors to educate people about health to help prevent illnesses before they even happen, not just current but also preventative medical care.
Sometimes that means educating the community on the need for real medical care instead of relying on witch doctors or overpaying inexperienced doctors for wrong diagnoses. It can also mean educating people about already existing government programs that are set up to help communities but that are often underutilized due to lack of public knowledge.
Health education can mean nutrition education, teaching people to eat the right kinds of food and treat their bodies well, helping them make permanent lifestyle changes that have long-term positive consequences. It means immunizations for preventable diseases rather than waiting to treat disease that has already broken out. Health education prepares the community to screen for treatable illnesses such as diabetes or high blood pressure. It can mean prenatal care as well, caring for babies before they are even born.
Sometimes health education is even as simple as teaching villagers to use latrines, wash their hands, and bathe with soap. What seems common knowledge in one culture can be almost entirely unknown in another. These simple changes can help eliminate preventable illnesses.