Palliative Care
Watch this 3-minute video on palliative care by Dr. Ashita Singh, EHA’s Director of Palliative Care
Palliative Care’s Significant Impact
If you or a loved one has ever needed hospice (or palliative) care, you know the enormous impact that service can have. Educating, reducing pain, helping the family—all of these things help ease a person toward death.
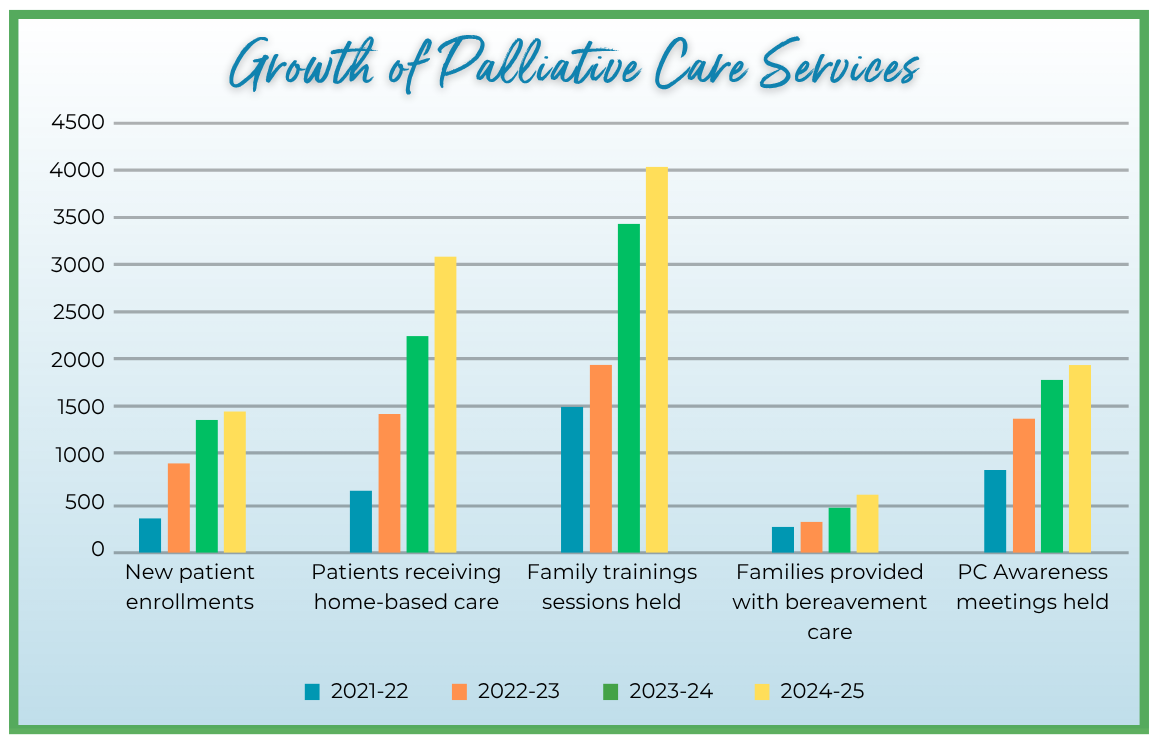
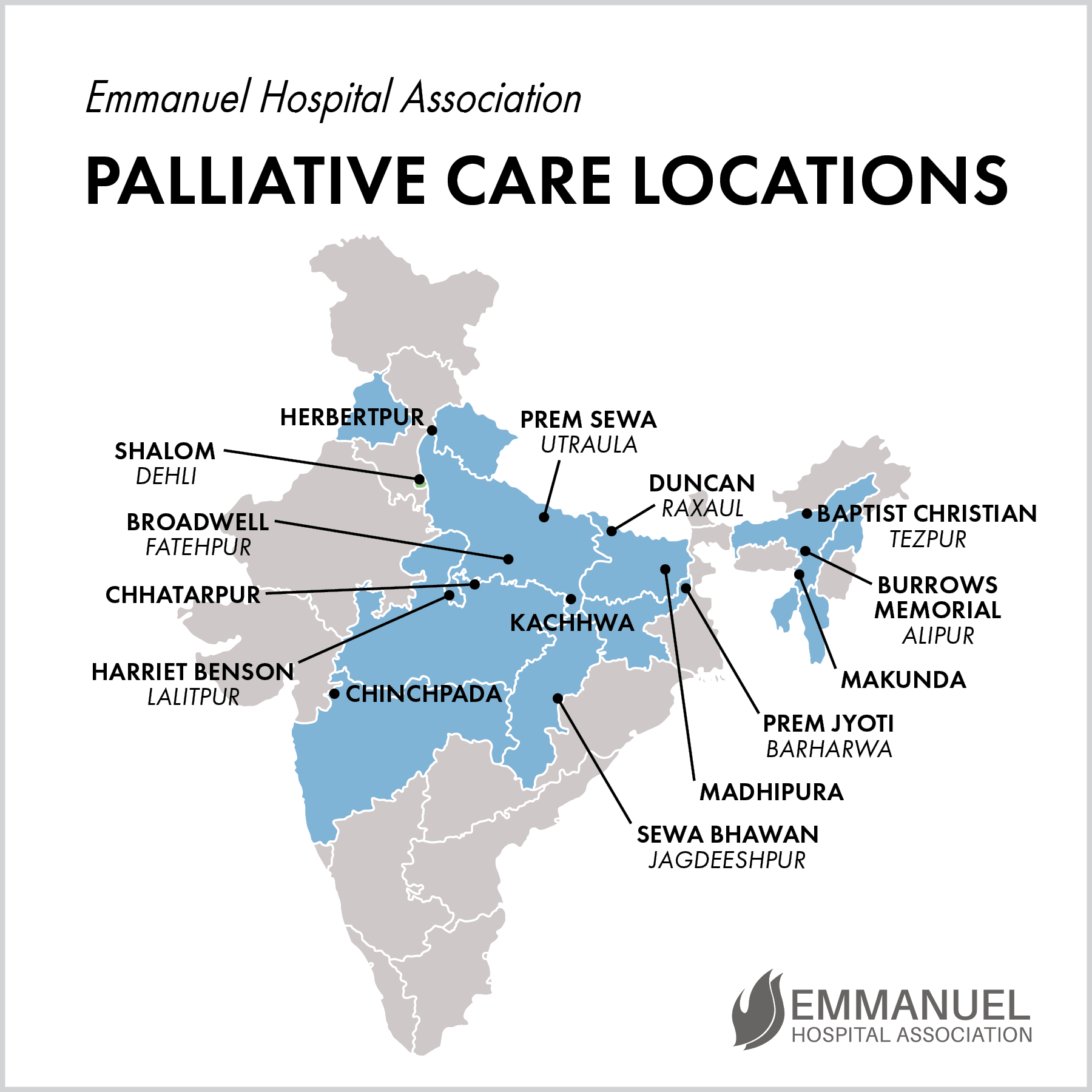
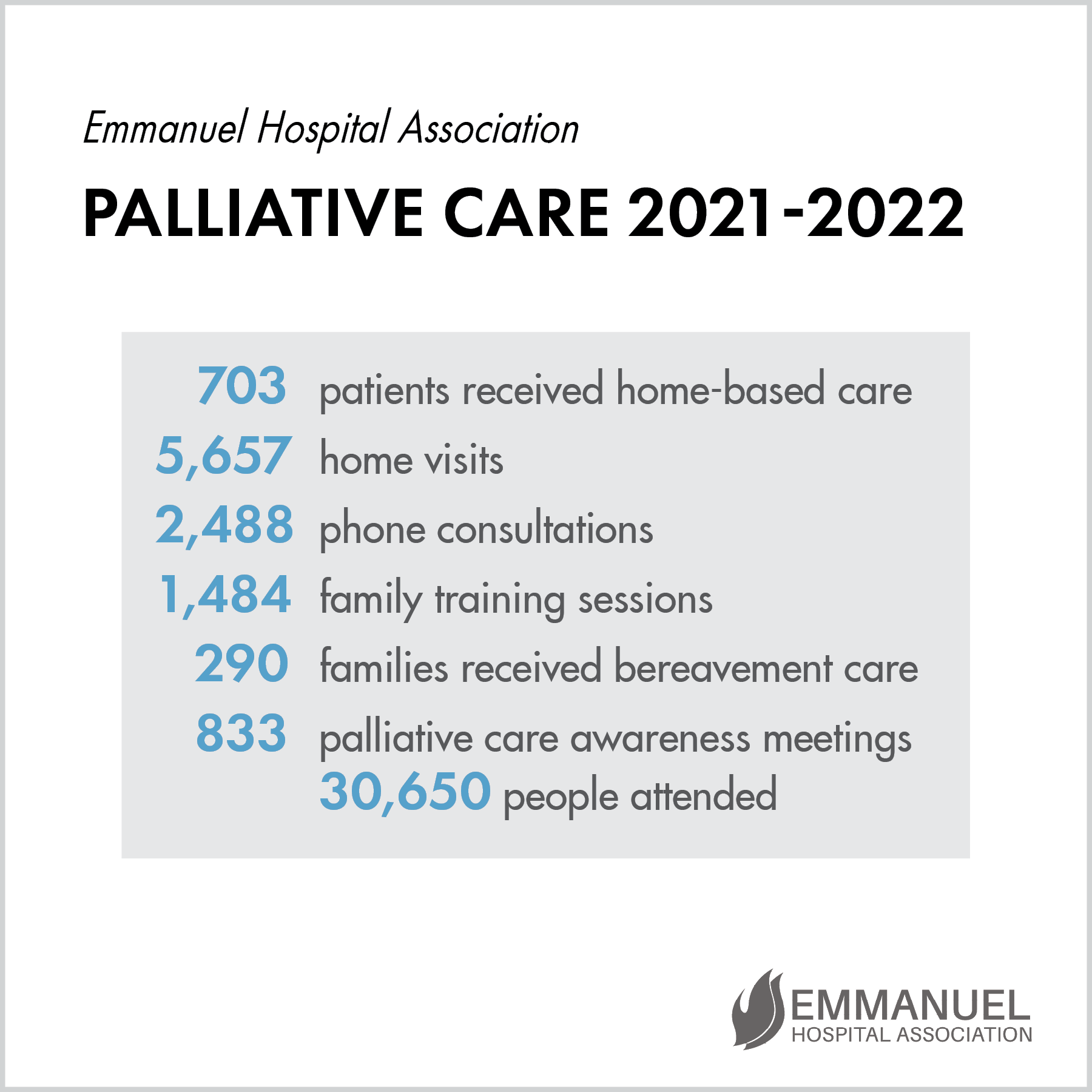
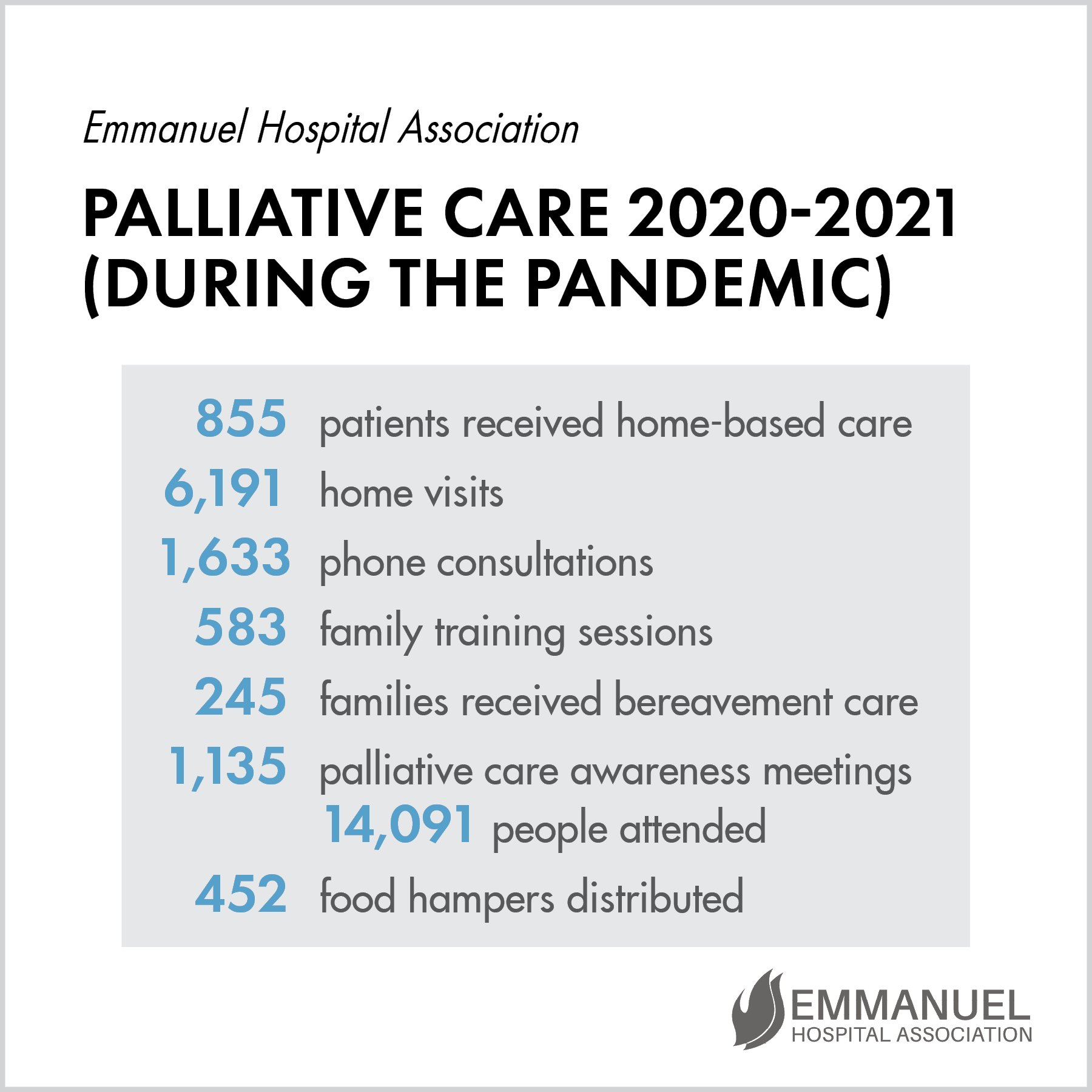
EHA’s palliative care’s impact is even more significant in areas where medical care is limited and funds are nonexistent. In just the last three years, the number of EHA’s hospitals with a palliative care team has grown from 11 to all 20. In addition to that, doctors and nurses across EHA are being trained to integrate the palliative care mindset into all areas of service in the hospital. This transforms how they deliver healthcare and makes them aware of patients’ needs so that care is holistic.
You can see from the chart above how much new patient enrollment and home visits have risen. You would be amazed to know how few staff accomplish all this work—and often get to patient homes by riding motor scooters on horrible roads, crossing treacherous footbridges and streams, and walking many miles. The staff members’ commitment to pouring out love and medical care on these patients is tremendous. Read on for a patient story that will touch your heart.
The Freedom to Weep
Arvind was suffering greatly until the Prem Sewa Hospital palliative care team found him. At just 33 years of age, he was dying from oral cancer.
The team was able to relieve much of his pain and dress his large facial wound, making him more comfortable. They taught Arvind’s wife, Suman, the best way to prepare his food.
In between caring for her husband and elderly mother-in-law, Suman goes to the nearby fields to work peeling sugarcane so that she can earn something for the family. The couple’s 12-year-old son went to live in the city with his uncle so he can earn money to send home. He washes cars and works in shops, and recently sent 13,000 rupees ($150), a huge sum, home to his parents.
Suman is so grateful for the support and the medication provided by the PC team. She was initially hesitant to learn how to dress his gaping wound, but with the gentle persistence and encouragement of the team, is now an expert. Suman said to the team through her tears, “If you had not been there to care for us, we would have had no hope. The only time I feel the freedom to weep and unburden myself is with you, because you take the time to listen to me.”
A Passion for Medical Missions
Conference challenges a new generation to put faith in action and serve the poor
Serving the poor of North India, EHA is part of a bigger global medical mission movement. That’s why we make it a point to participate in significant conferences designed to highlight the work done around the world. One such annual medical mission gathering in November is the three-day Global Missions Health Conference (GMHC) held in Louisville, KY.
The GMHC calls young medical professionals-in-training to consider serving the global poor. Thankfully, many have this vision and see themselves investing in medical work in difficult places. At the GMHC, presentations from frontline practitioners put a spotlight on critical needs which must be addressed, and bluntly chronicle the realities of serving day in and day out. Plenary sessions feature inspirational music and messages which vividly outline the need for more medical missions, and foster increased commitment from attendees. A range of medical mission personnel currently serving across Africa, Asia, and Central/South America make a point to be there, as do medical students considering future service. Young people can learn from veterans, and can explore opportunities for long-term placement, as well as medical residency options which fit future plans.
EHA’s head of palliative care, Dr. Ashita Singh, had an opportunity to present on our efforts in caring for suffering patients and the impact the work has on so many. She detailed EHA’s strategies to extend end-of-life assistance in rural north India, where it is virtually unknown. Launched more than a decade ago by veteran medical missionary Dr. Ann Thyle, the palliative program now touches patients and their families at all 19 of EHA’s locations. The model features home-based care by teams sent from the hospitals, and they served more than 2,000 patients last year, through 11,000 home visits. All told, the program touched the lives of some 50,000 people, many of them poor and marginalized with very limited access to quality healthcare of any kind, let alone palliative assistance.
As the EHA teams visit patients, they have opportunities to build relationships with family members and others in villages, bringing much-needed education about sickness and disease, and how to care for those in great suffering. Staff provide relief for patients who otherwise would be left to suffer and die alone and in agony. The default view of family members is that cancers and other life-limiting illnesses are untreatable and possibly contagious. Many are shocked that care is possible and available. What greater testimony of God’s love could be imagined than to bring this kind of help to those in such difficulty.
If your heart is particularly moved by what EHA is doing in palliative care, take time regularly to pray for the work. Beyond this, those with a particular interest in this arena are welcome to visit EHA and observe our palliative care efforts on the front-lines. This kind of experience could change your life! And of course, your help funding these efforts, which by their nature require constant support, would be most appreciated.
Until His Last Breath
Kab was a poor Muslim man who lived with his wife and three children in Chhatarpur. He worked for a trucking company for a very small wage.
Two years ago he discovered a blister in his mouth. A clinic referred him to a cancer hospital, but he had no money, so the sore went untreated. When he could no longer work, his wife did daily jobs so they could eat.
When Kab heard about Chhatarpur Christian Hospital’s palliative care services, the team helped him get a government benefits card. They sent him for treatment six hours away, but he could not be treated because of a low hemoglobin level. A member of the palliative care team donated blood so Kab could start chemotherapy.
After chemo, Kab grew weak and was admitted to Chhatarpur Christian Hospital. He was cared for until his last breath, and his financial needs were taken care of by the hospital, the palliative care team, and other palliative patients. Thanks to EHA, his children are getting an education and his family is receiving government benefits.
Palliative Care Services Expand
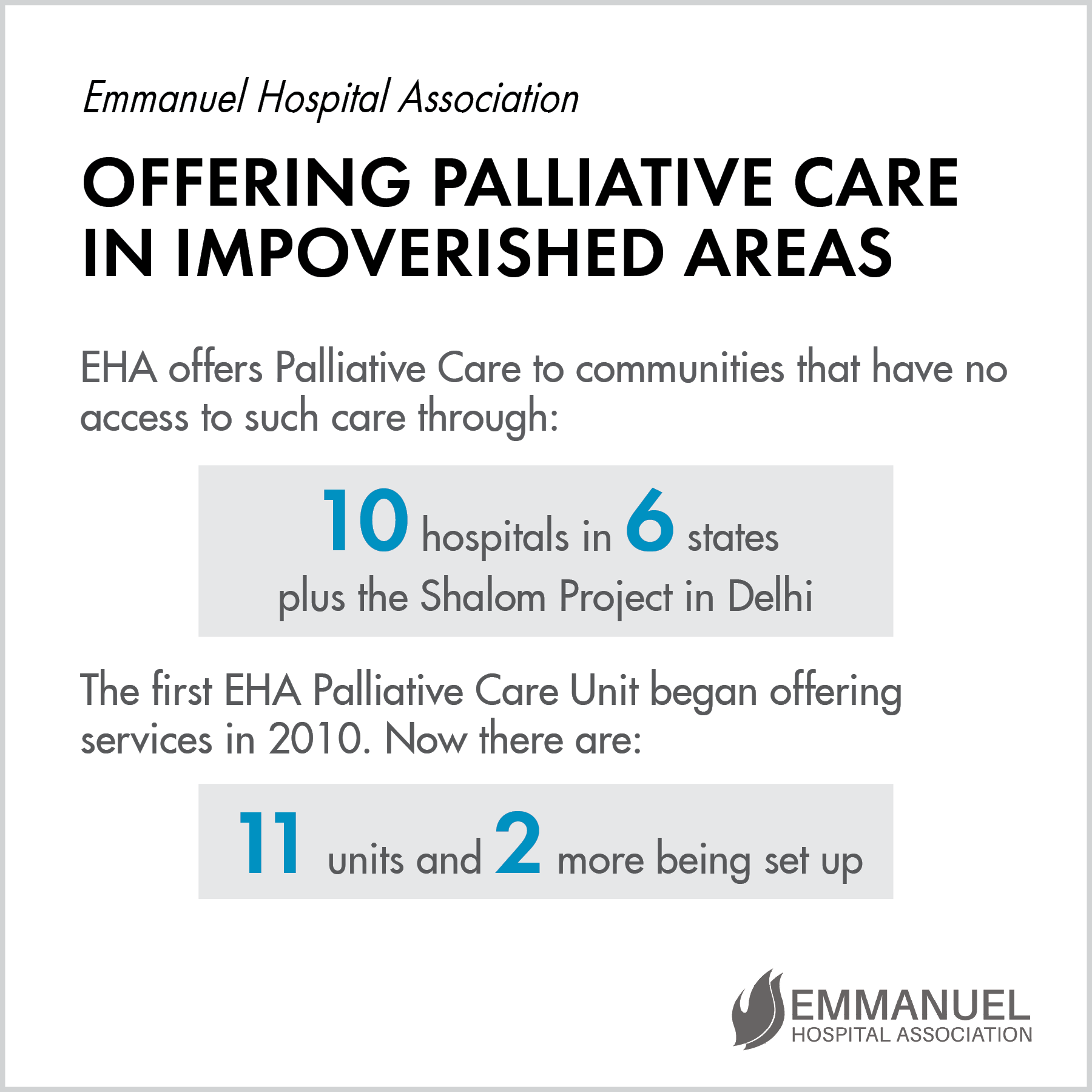
EHA’s palliative care services are expanding to two new locations at Chhatarpur and Barharwa. This means they now have 15 palliative care units serving at 14 hospitals and the Shalom Project in Delhi. EHA prioritizes caring for those with life-limiting illnesses, relieving their pain and bringing them dignity even as they suffer.
Palliative Care Teams Provide Holistic Treatment
While we may refer to end-of-life care as hospice in the US, in India it is called palliative care. Medical treatment and emotional support for patients with life-limiting illnesses is almost unheard-of in India, and EHA is doing its best to meet the needs around them.
The palliative care teams go where others will not, giving needed pain medication, dressing wounds, educating family members, and helping to ease patients on their way to “a good death.”
A New Lease on Life
When EHA palliative care teams go out into the field, they never know what they will find. When the team from Prem Sewa Hospital visited the home of a middle-aged woman with lung cancer, they were glad to see that she was still experiencing great relief from her breathlessness and pain because of the medication the team had provided. It was clear how much the family valued the visits by the team.
This woman has five daughters, and the staff discovered on this visit that one of the teenagers had a severe psychotic disorder for which she had received no evaluation or treatment. This young woman simply roamed the streets, completely unaware of her surroundings, while her family watched helplessly. The nearest place they could have taken her for treatment was four hours away, an impossibility for this impoverished family. The palliative care team was able to examine the girl in her home and prescribe medication for her mental illness. She now has a new lease on life.
Providing a Good Death
Salim had oral cancer and he was in excruciating pain. He knew he was in the last stages of his illness, but his last hope was to attend his daughter’s wedding.
He was brought to an EHA hospital for treatment because his wound was infested with maggots, increasing his pain considerably. The standard treatment of using turpentine-soaked gauze was not working because the infestation was deep in the tissue, so the palliative care team made a call to the coordinator to find another solution.
They consulted experts, searched books, and combed reference articles. The doctors found a recent publication that listed a treatment plan of Clindamycin, Ivermectin, and Albendazole to solve the problem, and the medications were started immediately. The team prayed for relief for Salim.
Within a few hours of starting this treatment, Salim began to feel much better as the medicine wiped out the infestation. The next morning, Salim was beaming from his hospital bed, filled with the hope of attending the wedding. The staff were jubilant at this dramatic transformation from heartrending moans to a brilliant smile.
Two days later, an extremely grateful Salim went back home, put on his best clothes, and joyfully attended the wedding celebration. He came back to the hospital later to thank the team for their loving care and prayer. He passed away peacefully a week later.
The palliative care team was touched as they realized once again the high value of end-of-life care that does not delay death, but does affirm human dignity. They care deeply about providing the highest quality of life to the very end, and they aim for a good death for everyone.
Palliative Care Alleviates Suffering
Restoring Dignity
The stories of EHA’s palliative care (PC) patients truly can be heartbreaking. The PC team at Harriet Benson Memorial Hospital was asked to travel to the home of a young man in his twenties.
Shivam had been addicted to smoking and alcohol and had never been to a hospital for treatment. He had a facial wound that was so disfiguring that it was impossible to make out where his features were. He stayed away from his wife, Meera, and two young children in a dark, dirty shack with no ventilation. When the PC team arrived, Sister Saroj cajoled Shivam into coming out so they could care for him. Slowly, he crawled out, and the team saw that he was reduced to skin and bones, with a large wound oozing on his face.
The team asked Shivam if he was ready for the bath that he only received when they visited, and he nodded eagerly. Gently, the doctor and nurses scrubbed his body and rinsed his face. The team trimmed his nails and combed his hair. They asked for clean clothes for him, but there were none to be had. The team asked Meera to wash his only shirt and then instructed her on how to dress his wound to contain the bleeding and discharge, and minimize the odor. They also taught Meera how to give Shivam the pain medication they had brought, and she took it gratefully, saying that it relieved his suffering significantly.
Sister Saroj then sat next to Shivam and spoke gently into his good ear, sharing that his dignity mattered and that they would pray for his relief and comfort. Tears welled in Shivam’s eyes as he gazed at the team and silently thanked those who had served him so graciously.
Persevering through Difficult Caregiving
Adjusting to the difficult situations they find themselves in can be very challenging for new palliative care team members. One nurse named Pari shared that at first, she could not tolerate either the sight or smell of illness, and she also struggled with severe motion sickness, even on short journeys. All of these issues made giving palliative care almost impossible, as the sights and smells are far worse than in hospital care, and the travel often involves many hours on bumpy roads. In the beginning, she often had nightmares because of the serious wounds she had seen, and she couldn’t get the odors out of her memory.
Undeterred, Pari asked God to help her overcome her weaknesses as she was eager to serve those who suffered without care. As she continued, she slowly overcame these hurdles and now is able to travel without motion sickness and can stand the worst sights and smells without flinching or experiencing nightmares.
Recently Pari and her team visited a young mother of two toddlers who has metastatic breast cancer. She was moaning in pan when they arrived, and she was suffering with excess fluid in her abdomen. The team was able to perform an abdominal paracentesis, removing 5 liters of fluid, which brought her much relief. Without nurses like Pari, patients like this one who cannot travel to a hospital would be left to suffer alone at home.
Palliative Care Teams Minister to Cancer Patients
At 14 of EHA’s hospitals, palliative care teams minister to those with life-threatening illnesses. The goals include improving quality of life and easing pain, as well as providing emotional and spiritual support.
At Broadwell Christian Hospital, they deal with oral cancer in about 50 percent of their cases. They find that these poor patients exhibit a lack of knowledge of the disease, a host of superstitious beliefs, cultural barriers, and a strong belief in faith healers, all of which makes their treatment and cure more complicated. Most of these faith healers give a 100 percent guarantee of a cure, which of course even cancer hospitals would not provide.
On top of the physical difficulties, cancer is viewed as a terrible omen, and people refrain from going near the patient. They are afraid of “cancer germs” in the air and don’t want to catch the disease. Education and cancer screening are key components of EHA’s palliative care teams’ efforts to combat this terrible disease. Watch a five-minute video to get a clear picture of what palliative care work in North India is really all about.
Palliative Care Teams Bring Hope to Sahana

Sahana is 42 and lives in a village near Chinchpada Christian Hospital. She has two small children, and her caring and supportive husband is a farmer with two acres of land for cultivation. Sahana had a happy and normal life until she fell ill two years ago. She developed a lingering fever and lost a lot of weight.
After seeking treatment at local clinics, she was referred to several hospitals in Mumbai. Despite numerous tests, the cause of her fever remained a mystery, and she returned home dejected and desperately ill. Squeezed dry of their life’s savings, the family could not afford more treatment. When homeopathic drugs and witchcraft failed, someone suggested that they try Chinchpada Christian Hospital.
When Sahana was brought to Chinchpada, she was mostly skin and bones, was unable to move, even in bed, and had a broken spirit. She would weep often and barely spoke or made eye contact. After evaluating her clinically, the staff started her on anti-tuberculous therapy. In light of her extreme sickness and guarded prognosis, she was enrolled in the palliative care program and put on bed rest at home.
The hospital assisted the family with financing her medicines and supported Sahana as she spoke of her feelings of desperation and hopelessness. With each passing week, Sahana’s health began to see improvement. As she ate better, she gained weight, her fever dropped, and she began to walk and become independent in her daily activities. When she came to the hospital for her appointments, she was always wearing a bright smile.
She and her husband now attend the local church regularly. Sahana attended the palliative care support group meeting last month and shared her story joyfully. With tears in her eyes she stood and thanked God for His mercy. All those who heard were blessed by her story. God brings Himself glory through seemingly hopeless situations.
Restoring Sanity, Sleep, and Appetite

by Dr. Honeysh George and Dr. Ann Thyle
Panchu, age 60, came to the outpatient department of EHA’s Kachhwa Christian Hospital. He was discovered in a nearby village by Mr. Sujit, a hospital community health worker. His head was entirely covered with a very dirty and foul-smelling towel that masked a large swelling on the right side of his face. It had been growing for the past two years. His eyes brimmed with tears as he shared about the constant intense pain that robbed him of his sanity, sleep, and appetite. He knew he had cancer, having been told at hospitals in Varanasi and Allahabad but, as is often the case in these villages, he refused treatment because of the exorbitant and impossible expenses for investigations and treatment.
When Dr. Honeysh went to meet Panchu at his home, he came to a small cow-dung covered courtyard of an old one-room mud hut. The dwelling accommodated Panchu’s wife, Godhna, one son, and four daughters. One daughter was married with three small children. Godhna and their daughter, Sita, worked seasonally on landowner’s fields, which was their only source of income. The family was just trying to survive, so cleanliness was the last thing on their minds. Apart from the general mess, the foul smelling drip from Panchu’s wound made it all the more miserable for the family.
Dr. Honeysh and Sujit spent time with Panchu, outlined his goals of care, provided pain medication, and dressed the wound. When they met him a few days later, Panchu said, “At last I can eat and sleep well without much trouble. If my pain was worth 1 rupee then, now it’s just worth 20 paise (1/5 as much).” There was great happiness and rejoicing among all of the family members. Although his wound is becoming larger and there is more discharge, Panchu is living almost pain-free, knows how to dress the wound himself, and looks forward to the doctor’s compassionate visits during which he is also supported spiritually. Much more work needs to be done to find ways to help this large family with better livelihood options and the opportunity for the younger children to attend school, but at least EHA is able to provide the best possible end-of-life care for Panchu.
Trying to Ensure a “Good Death”

by Dr. Ann Thyle
Mohammed (45) had advanced head and neck cancer, and spent his days and nights screaming in pain. Once EHA’s Palliative Care team found out about his situation and began to administer morphine, he found relief and was able to die at home, pain-free. This was a great comfort to his wife and four children in the midst of their grief.
Operating out of 14 hospitals and one project in Delhi, EHA’s palliative care services strive to improve the quality of care, affordability of services, and community engagement for those who are dying in the most neglected rural north Indian areas. EHA’s services attempt to incorporate the principles and components of a ‘good death’ as outlined by the End of Life Care Policy for the Dying. This includes having access to information and expertise, dying with dignity and privacy, providing pain and symptom relief, choosing the place of death and who is present, and having time to say goodbye.
Raghuveer (20) was cared for by the Palliative Care team of EHA’s Harriet Benson Memorial Hospital in Lalitpur, Uttar Pradesh. He and his family were kept well informed during the terminal phase. Raghuveer chose to die in the hospital with well-managed symptoms. Surrounded by his family, he died peacefully and painlessly after bidding farewell to his family and team members. Our Palliative Care teams’ goal is that a ‘good death’ will be the norm for all our patients.
According to a study of the status of palliative care in 80 countries, India ranked 67th with a very low score of 26.8%, with human resources, affordability of care, and quality of care being among the worst aspects. Provision of palliative care in India is poor with the positive exception of the state of Kerala in South India. Nationally, progress is slow and there are major shortages in specialists and facilities. Non-governmental organizations work to fill the gaps in public services. Subsidies vary across different states, and most state budgets fall far short of the significant needs. Excessive bureaucracy severely limits access to pain medication. On the whole, most terminally ill Indians are unaware of their palliative care options and do not benefit from pain alleviation prior to their deaths.
The Vicious Partnership Between Poverty and Sickness

by Dr. Ann Thyle
It has been rightly said that “poverty and sickness form a vicious partnership, each helping the other to add to the miseries of the most vulnerable in our country.” Different reports cite that 22 to 29 percent of Indians live below the poverty line. While the International Poverty Line is income less than $1.25 per day, and the US poverty line is less than $2 per day, the Indian poverty line is less than 27 rupees per day. This means that this huge group of people are each living on the equivalent of 40 US cents a day.
Who falls into this category? They are mostly tribal people, the Dalits (untouchables), and the labor class including farm workers in villages and daily wage earners in cities. Sixty percent of these people reside in the north Indian states of Bihar, Jharkhand, Uttar Pradesh, Chhattisgarh, Madhya Pradesh, Odisha, and Uttarakhand, since 85 percent of India’s tribal peoples live in these states. This is precisely where the hospitals of the Emmanuel Hospital Association are located, serving the communities with affordable health care, community programs, and palliative care, a service that is trying to contain and prevent household poverty.
Ram Swarup (54), a cancer patient cared for by the Palliative Care team at EHA’s Broadwell Christian Hospital in Uttar Pradesh, received free in-patient care, a blessing for this farmer who cannot work and whose family of six is being supported by the meager income from his only son’s daily wages.
Pinky (34) was also impoverished by futile cancer treatment, and is being cared for by the Palliative Care team of EHA’s Madhipura Christian Hospital in Bihar. When the team found them, her family of 11 was in extreme pain from hunger, the six children were unkempt, and her husband was overwhelmed as the only wage earner. The Palliative Care team was able to give sound and helpful advice on future treatment and possible government benefits they can access. They will also provide home care that will reduce treatment costs.
Illness Causes Destitution

by Dr. Ann Thyle
Gauri Shankar (28) lives in Budwar village, 10 kilometers from EHA’s Harriet Benson Memorial Hospital (HBMH) in Lalitpur, Uttar Pradesh. He lives with his wife Sudama (26), a daily wage laborer, their two school children, Kushboo (10) and Darshan (8), Gauri’s mother, and his mentally challenged brother, whose infirmity started ten years ago following a head injury from a physical fight with his uncle. The family was fairly well off farming five acres of land that allowed them to live in a good house and have sufficient food.
Everything changed in January 2015, when a blister on Gauri’s tongue was diagnosed as cancer after numerous visits to local practitioners. Later he underwent chemotherapy at the nearest Regional Cancer Center. The family sold all their land to meet medical costs and began trying to survive on Sudama’s wages alone. When the Palliative Care team of HBMH visited Gauri’s home, they found a completely destitute family existing on one meal a day, the children withdrawn from school and in torn clothes—a truly pitiable state brought on by the unexpected illness of the main wage earner.
The team now provides monthly food supplies for this family and will open a tea shop that Gauri can run for as long as he is able. They are also exploring how the children can return to school. Without such efforts, numerous rural families are pushed into a degree of poverty from which it is impossible to emerge.
Training Link Nurses Improves Care

by Dr. Ann Thyle
Chhatarpur Christian Hospital, a 150-bed facility, has provided compassionate care to the people of Chhatarpur and the surrounding villages for more than 80 years. The total population of the district (like a county in the US) in the 2011 census was 1,762,857 with just 64.9% literacy. The villagers are socially and economically backward, with little knowledge about healthy lifestyles or access to good quality healthcare.
Started in 1930 as the Elizabeth Jane Bell Stephenson Memorial Hospital, Chhatarpur Christian Hospital presently has a staff of 182, of which 74 are nurses, 8 are doctors, and 1 is a dentist. It also runs a School of Nursing and a vibrant Community Health and Development Project.
The Palliative Care service was started in May 2014, supervised by a trained nurse with a master’s degree and run on a daily basis by two nurses trained by the Indian Association of Palliative Care with valuable input from the Community Project manager. Although it is mainly a home-based care service, doctors are available for inpatient and outpatient care. Tutors from the Nursing School assist in practical family training. Large-scale awareness programs are held in village communities and schools with village leaders. Some of the initial comments we received, such as, “Please start this service as soon as possible,” “This is the first time we have heard about such an opportunity for the terminally ill,” and “If a person has cancer, he will die anyway” have now been dispelled by sharing information and providing subsidized care.
Since the inpatients are scattered in different hospital wards, a ‘Link Nurse’ training program was initiated whereby senior ward nurses had a three-day training session in palliative care. This model was first piloted at EHA’s Baptist Christian Hospital in Tezpur, Assam. The goals are:
- To improve palliative care provision within the hospital
- To improve links between the palliative care staff and the nurses serving on the wards
- To equip nurses with knowledge and skills that can help them to provide care to patients admitted on the wards
- To distribute and use clinical protocols
- To use a categorization system for patients
Our hope is that improving accessibility to palliative care in a large hospital through Link Nurses will improve care, and that knowledge about palliative care will increase in the hospital so that more patients will have access to this service.
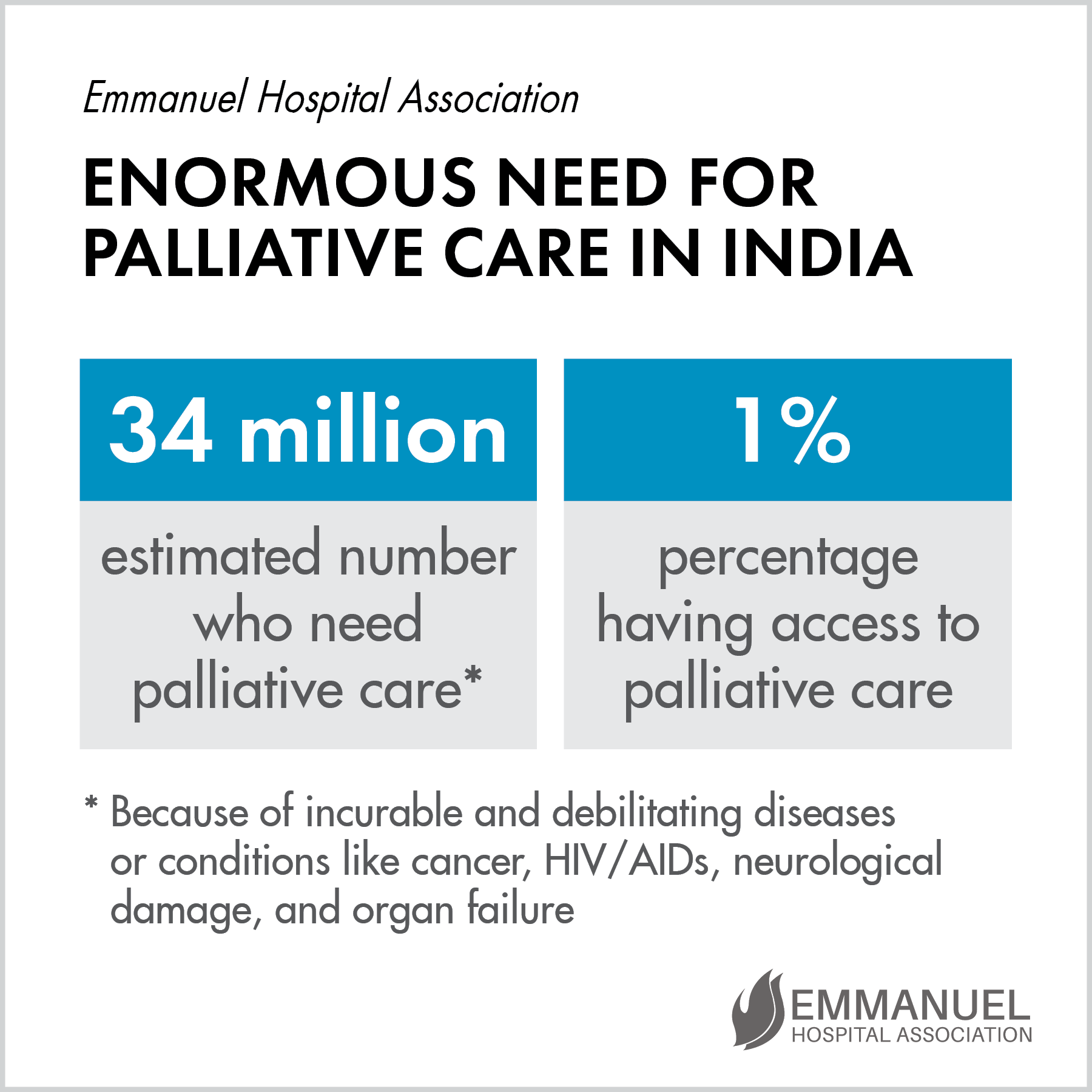
Bringing Dignity to the Dying

Palliative care isn’t something people want to think about – until one of their loved ones desperately needs it. Also called hospice or end-of-life care, palliative care is designed to make patients comfortable in their last days. In the United States, patients often have multiple options for this type of care. But in India, the options just aren’t there. Palliative care is almost non-existent in rural North India where medical cures are often impossible because patients wait too long to seek treatment, or have limited treatment options, or just live with extreme poverty. Less than one percent of the 34 million people who need such care have access.
Into this bleak situation came EHA. After two years of prayer, Dr. Ann Thyle developed a palliative care program at Harriet Benson Memorial Hospital in 2009. She began with just one nurse and a desire to treat the whole person – emotionally, socially, spiritually, and physically. They sought out the terminally ill in numerous villages and found that dying patients often are filthy, in pain, and alone. There is such a social stigma for those who are ill that few will admit to having sick relatives. Only after holding awareness meetings about serious illness in the villages do people start to share that they know someone in that type of situation.
Typically, when a person is diagnosed with cancer in India, they go to a cancer center where they are told to pay $2,000 for 6 chemo treatments. These people make $1 a day just to support their families, so there is no way they can pay this amount. The person just goes home to deteriorate and die. The rest of the family must keep working to meet basic needs, so the patient is left on his or her own. Families have no idea how to bathe, dress wounds, and otherwise care for their sick loved one. The palliative care team comes in and teaches the family how to do these things and also provides pain relief in the form of medication. They bring dignity to these patients’ last days.
Physical and Spiritual Needs Met

She came to the outpatient department of Broadwell Christian Hospital (BCH) with uncontrolled bleeding. The diagnosis: cervical cancer.
Fifty-eight-year-old Kusum Pandey went on to have major surgery at another hospital as well as some radiation treatments, but soon the doctors told her there was nothing more that could be done. When she returned home, the Palliative Care Team at BCH took over her care. Providing symptom relief and pain management, the team was able to care for her physical needs. Because of this, they had the opportunity to share God’s love with her and address her spiritual needs as well. Her family appreciated the prayer support, and doors are open to further communication.
Relieving Pain and Suffering

She couldn’t even straighten her body to lie flat due to severe abdominal pain. Kamala Jain had cancer of the gall bladder and had been treated at another hospital and given morphine for the pain, but it wasn’t working. Realizing that she wasn’t absorbing the morphine, the Palliative Care team added two other medications, and within 24 hours, she was able to lie flat and even regained her appetite. Due to the advanced stage of her disease, she died peacefully at home a week later.
Care for the dying and terminally ill is rare in North India. In the state of Uttar Pradesh alone, which numbers 200 million people, EHA provides the only home-based palliative care programs. The needs in this area are huge. Focusing on relieving debilitating pain and preventing the suffering of patients, palliative care deals with both chronic illness and life-ending situations. The Palliative Care teams seek to improve the quality of life for suffering patients by providing medical, emotional, and spiritual support.
Palliative Care Team Brings Hope

Practical help from the Palliative Care team takes many forms. They provide food and hygiene products for six months for the most needy families who lose their main wage-earner. Income generation is often at the forefront of families’ minds when they lose a parent. So a small tailoring center was opened to teach relatives to acquire sewing skills in order to bring home much-needed pay. Older children attend this center, and when they reach a certain level of proficiency, the Care team gifts them with a sewing machine and helps them set up their new venture.

One family taking advantage of this sewing training lost their 30-year-old husband and father to tongue cancer. Before he died, Rameshwar Prasad begged the members of the Palliative Care team who were treating him to take care of his wife and four children. His wife has since been employed as a cleaner at an EHA hospital, his sons have been enrolled at a boarding school to receive a high quality education, and his older daughter is enrolling in the tailoring classes so she will have skills to add to the family income.

Another man, Nanhe Das, received help of a very different kind. The team discovered him — paralyzed, filthy, and despondent. They cleaned him up and brought him to the hospital for medical, emotional, and spiritual support. Then the Palliative Care team went to work to complete paperwork, obtain needed signatures, and pick up a hand-propelled tricycle that he can drive with his arms. The mobility this will provide him is priceless.
While providing such practical help, the Palliative Care team can also share the love of God to bring real hope to these struggling people.
Pain and Death are Erased

Fifty-year-old Kalideen came to Broadwell Christian Hospital howling in pain. His family was in tears as they watched him struggle. As the story unfolded, the medical team learned that Kalideen had been a successful police officer wielding a lot of power and status. But wealth and prestige cannot keep cancer away.
Kalideen had been diagnosed with pancreatic and lung cancer which spread to his spine two years before. He was started on chemotherapy at one of the best institutes in the country. Eventually, he was told there was nothing more the doctors could do to stem the cancer’s spread. He went home and began taking over-the-counter medications to deal with the pain, but eventually his agony was so great he asked to be taken to the hospital.
The Broadwell doctors immediately assessed his condition and administered morphine and some other medications to relieve his suffering. After ten days, his condition stabilized and he was discharged. Kalideen was exhausted and discouraged, and he wanted to die. His greatest concern was his three unmarried children, and he felt hopeless. So the Palliative Care Team visited him as often as they could. Over a period of time, they watched his countenance change. He went from being an angry, growling man to being remarkably calm and composed. The team often prayed with Kalideen and his family and read them verses of comfort.
As the Palliative Care team began to see changes in Kalideen indicating that he was nearing the end of his life, they gathered his family around him. The team encouraged them to speak to Kalideen and reassure him of their love. He soon peacefully breathed his last. The Palliative Care team went to his house the next day and proceeded to the funeral as well. Kalideen’s sons thanked the team for being there for them in the most difficult of times. The Palliative Care team was glad that they were able to ease his suffering and hopelessness at the end of his life.
Skeptical Patient Experiences Turnaround

He was 42, married, a member of Bundelkhand Christian community, and gainfully employed as a market executive. But that didn’t stop cancer from striking Manish Das. He had a habit of chewing tobacco, and he developed a lesion on his tongue. Manish had surgery at a cancer hospital to remove the malignant tissue and had follow-up chemotherapy and radiation.
A month later, Manish told his doctor that he had an ulcer on his left cheek but was told that it was just a side effect of radiation that would heal eventually. Instead, it grew worse.
The Chhatarpur Christian Hospital Palliative Care team was put in touch with Manish, and they visited him in his home. Initially, he was very skeptical toward the team and did not want to follow any of their recommendations. He even recorded their conversations on his cell phone. But when he went to his doctor and played the recordings, his doctor applauded the Palliative Care team.
Humbled and weary, Manish spoke with the Palliative Care team once again. He had pain and difficulty in swallowing, and was unable to talk properly so he had lost his job. His cancer spread, and the team assured Manish that they were always available to guide and help him in any way possible. His church family also came to pray with him and support him.
As Manish’s condition worsened, the Palliative Care team treated him and showed his family how to care for him. They encouraged him to restore his relationships with both God and men. In the end, Manish and his family were grateful for all of the team’s care. When he passed away at Chhatarpur, the Palliative Care team continued to support his family in their grief, and the local church members now have a very positive opinion of Chhatarpur and its ministries.
Dignity in Life and Death

Suman was only 23 when she found a lump in her breast. She was currently breastfeeding her second child, so she didn’t think much about it, went to a local doctor, and took the two-week course of medicine he prescribed.
When the lump didn’t disappear, she went to a doctor in another city who also gave her medicine and told her to come back if it didn’t help. When she finally returned to the hospital, the biopsy they performed showed that she had cancer. It was so advanced that it was inoperable, but she underwent six cycles of chemotherapy.
By the time GM Priya’s Palliative Care Team found out about Suman, she was at home and in such severe pain that she was unable to sit up or talk. They gave her an injection for the pain, and when she was able to speak, she asked them why she was sick and if she would get better. She told them about her two young children. At this point, her left breast was rock hard, oozing pus, and throbbing with pain. She also had a lump in each armpit, indicative of cancer in her lymph nodes.
Because her husband and other family members were indifferent to her condition, the team spoke to Suman’s brother about the severity of her medical situation and the futility of treatment. They promised to provide palliative care for Suman and relieve her pain. Despite the team advising against it, her brother took her to one more hospital in the hopes of a different diagnosis, but the doctors there sent her home too.
When the Palliative Care team visited Suman after her return, they found her on a cot in the back yard, breathless and in excruciating pain. Her in-laws had moved her out of the house in the hopes that she would die more quickly. Suman had not slept for several nights, her gown was stained with blood, and she could barely talk.
The team consulted her brother, and he agreed that she should be brought to GM Priya for palliative care during her last days. The staff cleaned her wound and gave her pain medication, and then she wanted to talk about her worries and fears over her children, age six and three. She took the news of her prognosis bravely, and said she was not afraid of death. In the three weeks she remained at the hospital, she forged a special bond with each staff member, and kept up her spirits without complaint even amidst great discomfort.
Whenever a staff member went to visit Suman in her bed, she would ask about their well being before they could inquire about hers. When they choked up over her condition, she would hug them and tell them not to worry about her. The team prepared her family for her passing, and they came to visit often, bringing her children. Suman passed away peacefully, surrounded by family, and both her brother and husband were immensely grateful for the care she had received at the hands of GM Priya’s Palliative Care team.
Suman’s life and passing are not only a palliative care success story, but also a lesson for each staff member who learned so much from the caring, gentle woman who was brave to the very end.
Dependent No More

Seema was only 19 when she went to get some mud to repair her katcha (mud) house and a huge rock fell on her back. She was unable to get up. Her brother took Seema to several hospitals, but all the doctors said the same thing—she was paralyzed and would never walk again. Forced into dependency on her mother and brother, Seema spent her days on a small bed feeling useless.
While conducting awareness sessions in Seema’s village, the Palliative Care team from Harriet Benson Memorial Hospital heard about her situation. Going to visit, they enrolled her in palliative care and sought to find her some means of making an income. Since Seema knew how to tailor, the team gave her a sewing machine. Thrilled with her new tool, Seema is now able to support herself by making kurtas and dresses to sell. Reaching out to the hurting and finding solutions to their problems is just one way EHA teams show love and make a difference in other’s lives.

About EHA’s Palliative Care Projects
Palliative (hospice) care is an area of healthcare that focuses on relieving pain and preventing unnecessary suffering of patients, whether the diseases are chronic or life-ending. In India, with recent improvement in standards of living, disease patterns are changing. Life-limiting diseases, such as cancer, HIV/AIDS, and heart disease are increasing. Despite this transition, there are 19 states and union territories in India where there is no evidence of palliative care. In 2010, EHA began the only home-based palliative care program in the state of Uttar Pradesh, which numbers some 200 million people. The needs are overwhelming, but the staff press on.
The program’s main goal is to work with families to improve the quality of life of the patient by relieving pain, managing distressing symptoms, and providing psychological, social, and spiritual support as much as possible in the home environment. The practical implications vary from patient to patient and include help with income generation and programs for the children. Through the varied means of assistance the Palliative Care team is able to provide for individuals, they are helping one person at a time. And as they share essential medicines and provide sensitive care, they are also able to share about God, bringing hope to the suffering and dying.